
Best adjuvant (assist) for chemotherapy | 1+1>487% |
Effectively improve chemotherapy effect, treatment, immunity.
Reduce side effects and recurrence.
Overview / Relation / Abstract / Role / Principle / Action / Mechanism / Function / Work |
Neuroblastoma - Childhood: Latest Research
Abstract / Summary / Overview of Apoptosis.
Why do cells undergo apoptosis?
The relationship between cancer cells and apoptosis.
Where are the weaknesses and symptoms of cancer cells?
Are cancer cells aggressive?
Extraordinary Solamargine (Role, Principle, Action, Mechanism, Function, Work)
Solamargine's major function mechanism:
Solamargine vs cancer
Best Chemotherapy Adjuvant. (1+1>478%)
Effectively improve chemotherapy effect and cure.
When cancer cells are less resistant to drugs, chemotherapy becomes more effective.
Extract : https://www.cancer.net/cancer-types/
Neuroblastoma - Childhood: Latest Research
You will read about the scientific research being done to learn more about neuroblastoma and how to treat it.
Doctors are working to learn more about neuroblastoma, ways to prevent it, how to best treat it, and how to provide the best care to people diagnosed with this disease. The following areas of research may include new options for patients through clinical trials. Always talk with your child’s doctor about the best diagnostic and treatment options for your child.
Many of the items below are explained earlier in this guide's Types of Treatment section. Additional studies are underway to improve the use and effectiveness of current treatments, as well as to find new approaches to treating neuroblastoma.
New drug combinations. Clinical trials are underway to study the use of chemotherapy combined with immunotherapy, tyrosine kinase inhibitors, or other drugs. Researchers hope that these drug combinations will increase the effectiveness and decrease the side effects of induction treatment.
Stem cell transplantation. A Children’s Oncology Group clinical trial comparing 2 cycles of high-dose chemotherapy to 1 cycle of high-dose chemotherapy and stem cell transplantation has recently been completed. Patients who received tandem cycles of high-dose therapy had improved event-free survival. Based on these results, the Children’s Oncology Group now considers 2 cycles of high-dose therapy with stem cell transplant the new standard of care for high-risk neuroblastoma patients. A European study compared the results for children who received conditioning prior to a stem cell transplant with carboplatin, etoposide, and melphan as compared to busulfan and melphalan. The study suggested that the outcome was better for children treated with busulfan and melphalan.
Targeted radiation therapy. Treatment with a high-energy form of radioactive iodine (I-131) with MIBG has been shown to have the tumor respond in about 30% of patients with recurrent or refractory neuroblastoma. This treatment is currently only available at certain cancer centers in the United States. Recently completed New Approaches to Neuroblastoma Therapy (NANT) clinical trials testing radioactive MIBG alone or combined with radiation sensitizers have shown higher response rates when MIBG is combined with vorinostat. Other NANT studies are testing MIBG combined with dinutuximab, and there are plans to amend this study to test vorinostat combined with MIBG and dinutuximab. The Children’s Oncology Group is conducting a randomized phase 3 study evaluating the efficacy of adding radioactive MIBG to the induction regimen in newly diagnosed patients with a high-risk neuroblastoma. Other radiopharmaceutical therapies that are being evaluated include 277 (277Lu)‐DOTATE and astatine‐211 (211At)‐mIBG.
Molecular targeted therapies. Research on the use of small molecules to target the cell functions that are abnormal in neuroblastoma cells is ongoing. Lorlatinib, and other drugs that inhibit ALK, a tyrosine kinase that is mutated in a subset of neuroblastomas, as well as other tyrosine kinase inhibitors are being tested in clinical trials. Other treatments currently in phase 1 or phase 2 studies include bromodomain and extra‐terminal motif (BET) bromodomain inhibitors (for their inhibition of MYCN). Aurora kinase inhibitors have also been combined with chemotherapy for the treatment of neuroblastoma.
Biomarkers. New tools are being developed to help find out the clinical aggressiveness of the tumor and response to treatment that may be used in the future to tailor therapies to individual patients. These include the use of circulating tumor DNA for genomic and epigenetic characterization of tumors and for determining how the tumor will respond to treatment. Learn more about tumor marker tests.
Imaging techniques. New imaging approaches, such as FDG‐PET‐MRI, 124I‐mIBG PET‐CT, or 68Ga‐DOTATATE, are being evaluated to see how they may help patients with neuroblastoma in the hope that these newer scanning methods may lead to more precise tumor localization.
Palliative care/supportive care. Clinical trials are underway to find better ways of reducing symptoms and side effects of current neuroblastoma treatments to improve comfort and quality of life for patients.
Abstract / Summary / Overview of Apoptosis.
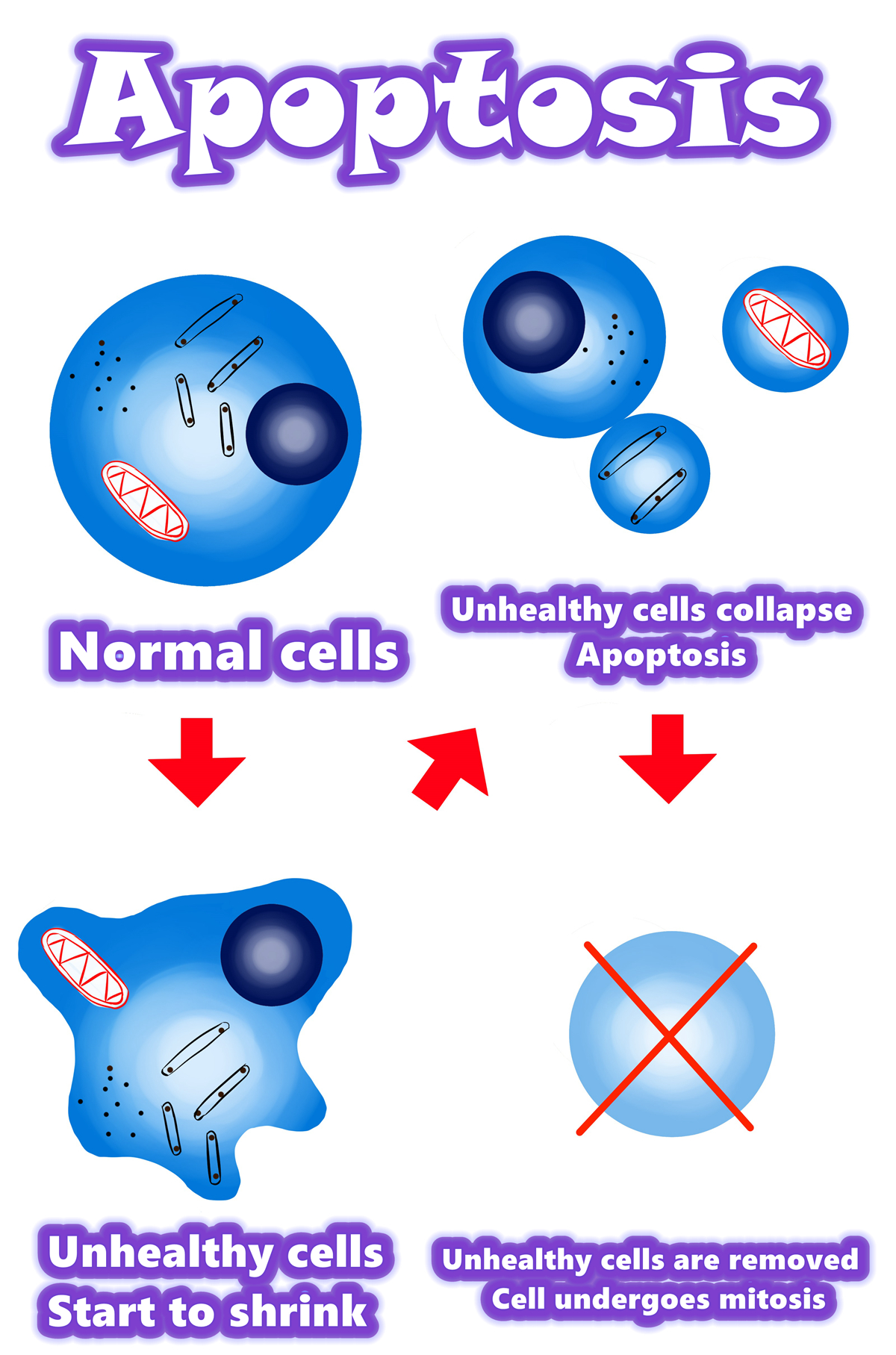
Overview of apoptosis
•Programmed cell death
•Apoptosis is a form of programmed cell death, or “cellular suicide.”
•Apoptosis is different from necrosis, in which cells die due to injury.
•Apoptosis removes cells during development, eliminates potentially cancerous and virus-infected cells, and maintains balance in the body.
Why do cells undergo apoptosis?
- Basically, apoptosis is a general and convenient way to remove cells that should no longer be part of the organism.
- Some cells are abnormal and could hurt the rest of the organism if they survive, such as cells with viral infections or DNA damage.
- Apoptosis is part of development
- In many organisms, programmed cell death is a normal part of development.
The relationship between cancer cells and apoptosis
Apoptosis can eliminate infected or cancerous cells.
When a cell’s DNA is damaged, it will typically detect the damage and try to repair it.
If the damage is beyond repair, the cell will normally send itself into apoptosis, ensuring that it will not pass on its damaged DNA.
When cells have DNA damage but fail to undergo apoptosis, they may be on the road to cancer.
However, “successful” cancer cells successfully evade the process of apoptosis.
This allows them to divide out of control and accumulate mutations (changes in their DNA).
Apoptosis is key to immune function
Apoptosis also plays an essential role in the development and maintenance of a healthy immune system.
Where are the weaknesses and symptoms of cancer cells?
The symptoms of cancer cells are in the nucleus.
The nucleus controls the outer cytoplasm, cell composition, cell viability, etc.
DNA mutations also mutate in the nucleus.
Therefore, to treat cancer cells, we must first enter the nucleus.
Let the “regulatory cell gene” mechanism enter the nucleus to regulate
Are cancer cells aggressive?
After the action of Solamargine, the aggressiveness of cancer cells is alleviated.
So after using Solamargine, many patients feel that I am half better.
Although the tumor does not disappear quickly, patients feel that the degree of aggressiveness is reduced.
Extraordinary Solamargine (Role, Principle, Action, Mechanism, Function, Work).
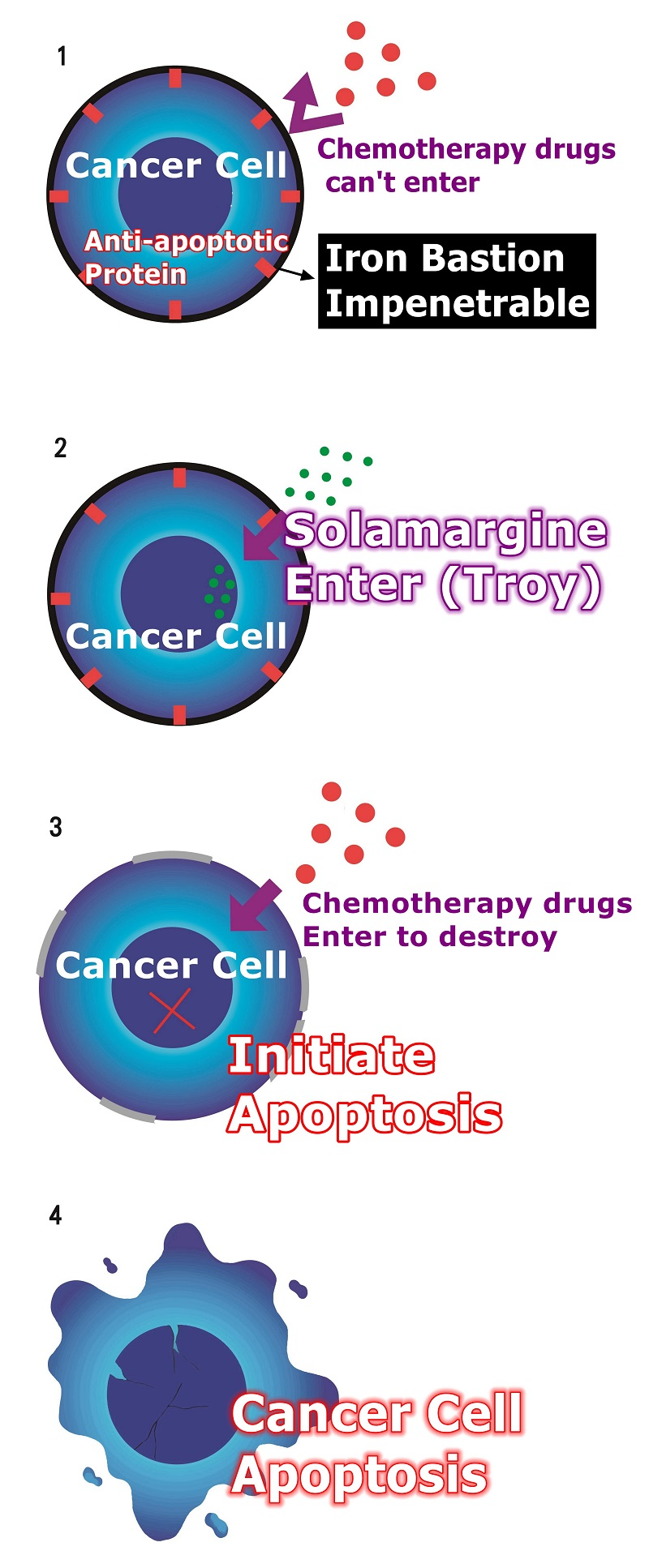
Solamargine's major function mechanism:
When Solamargine enter,
Solamargine activates receptors that are turned off by cancer cells, allowing cancer cells to modulate again.
Solamargine modulates the anti-modulates genes of cancer cells, making cancer cells less resistant.
Reduced drug resistance
When cancer cells are less resistant to drugs, chemotherapy becomes more effective.
Solamargine modulates the mutated genes in cancer cells and then initiates cancer cell apoptosis to achieve anti-cancer effects.
Solamargine combined with which chemotherapy drugs are more effective in treating cancer cells?
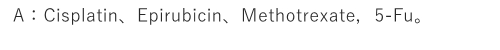
Solamargine vs cancer
Solamargine vs cancer
The picture shows the death of cancer cells.
The black and black parts are cancer cell nuclei.
Even if the nucleus ruptures, the cancer cells will die.
The figure shows that cancer cells can cause death.
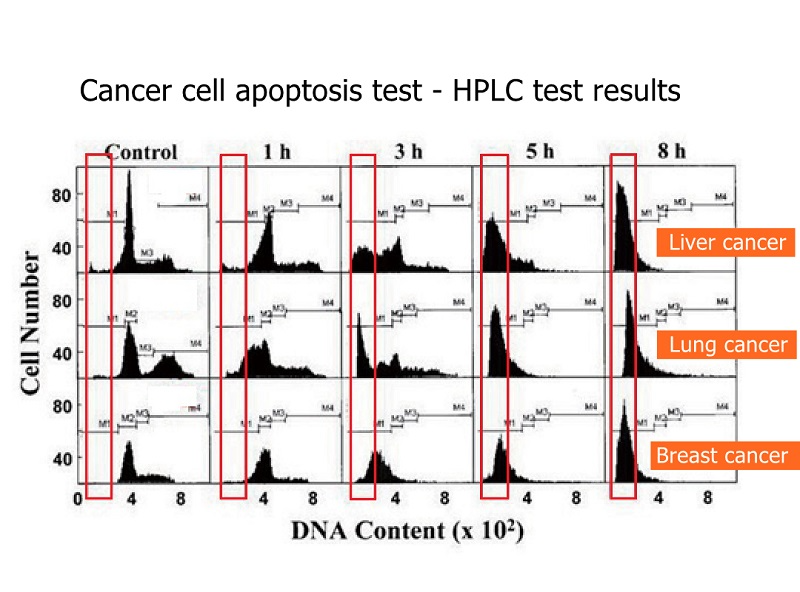
The figure shows that cancer cells can cause death.
The figure shows that the death of lung cancer cells is relatively slow, and it will not be obvious until eight hours later.
The figure shows that the death of liver cancer cells is very obvious, even more obvious in eight hours.
The graph shows that breast cancer cells die faster. It was obvious from the beginning that breast cancer is easy to treat, and patients with breast cancer need not worry.
Best Chemotherapy Adjuvant. (1+1>487%)
Effectively improve chemotherapy effect and treatment.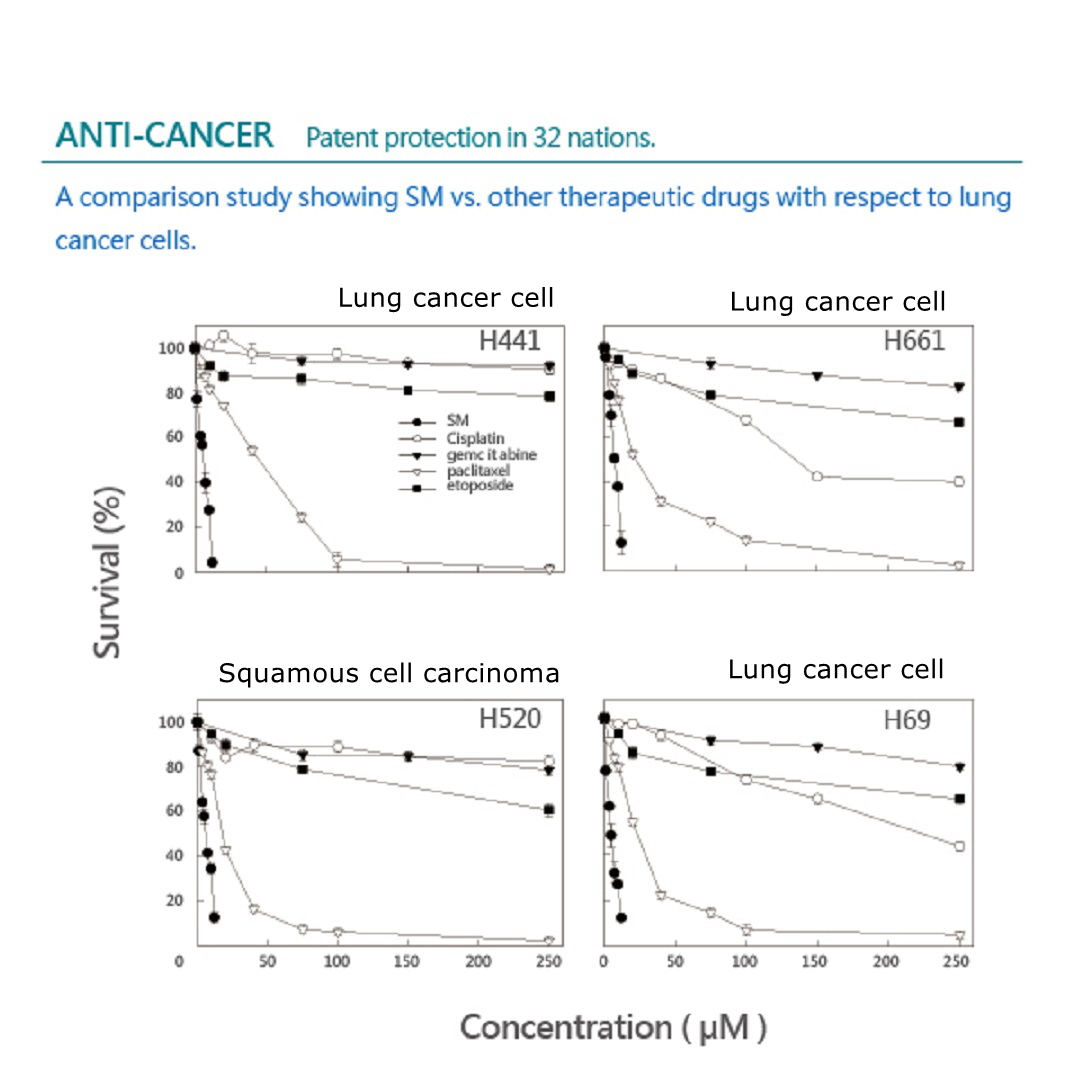
ANTI-CANCER
Patent protection in 32 nations.
A comparison study showing Solamargine vs. other therapeutic drugs with respect to lung cancer cells.
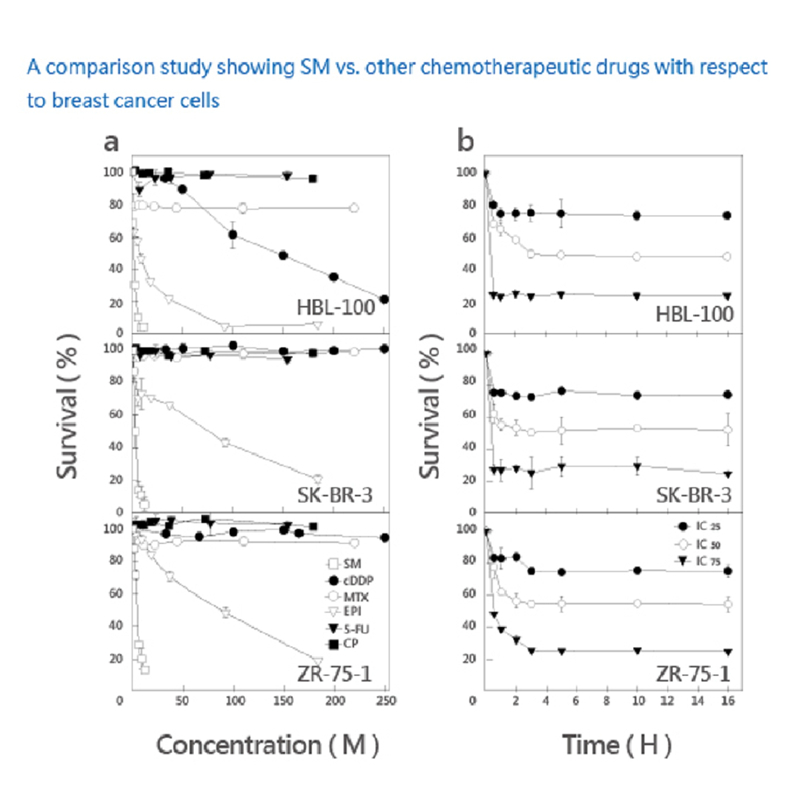 A comparison study showing Solamargine vs. other chemotherapeutic drugs with respect to breast cancer cells.
A comparison study showing Solamargine vs. other chemotherapeutic drugs with respect to breast cancer cells.
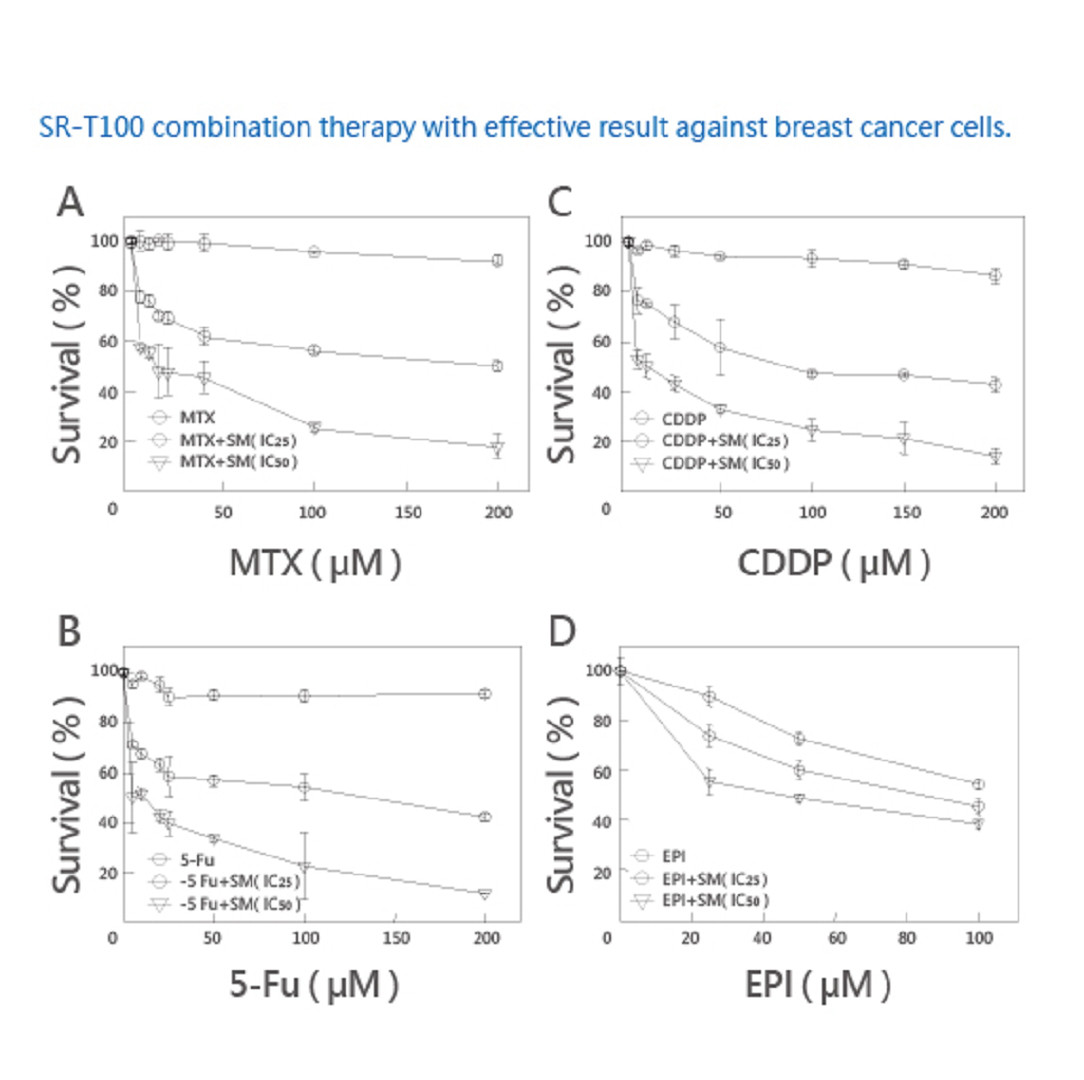
SR-T100 combination therapy with effective result against breast cancer cells.
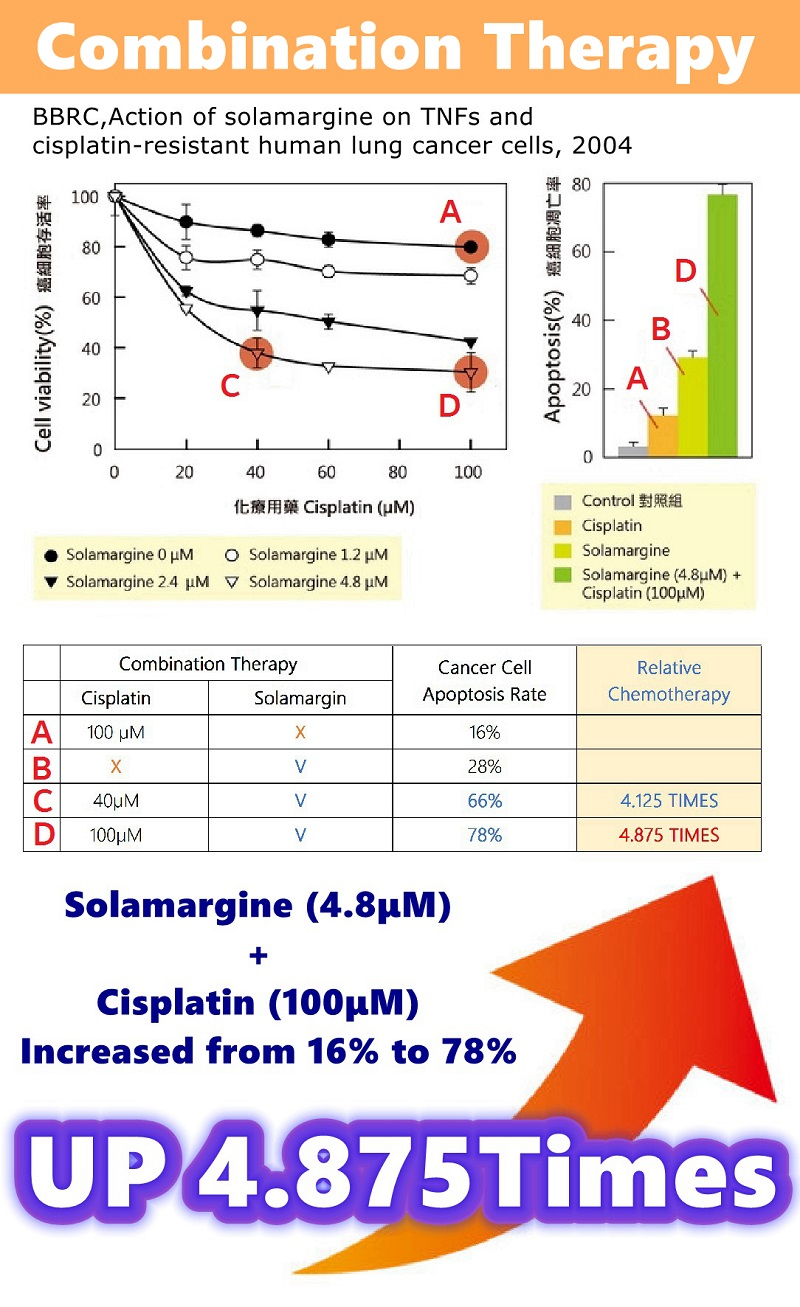
Combination Therapy | Research results for lung cancer cells.
A. Chemotherapy (100μM), 16% of cancer cell apoptosis.
B. Alone SM (4.8μM), 28% of cancer cell apoptosis.
C. SM (4.80μM) + Chemotherapy (40μM), 66% of cancer cells apoptosis.
D. SM (4.80μM) + Chemotherapy (100μM), 78% of cancer cell apoptosis.
SM has a clearing effect better than Chemotherapy.
The combined treatment of Solamargine and Chemotherapy significantly increased the apoptosis of lung cancer cells.
SM (4.8μM) + Chemotherapy (40μM), increased from 16% to 66% (up to 4.125 times).
SM (4.8μM) + Chemotherapy (100μM), increased from 16% to 78% (up to 4.875 times).
Reorganized from: BBRC. Action of Solamargine on TNFs and drug-resistant human lung cancer cells 2004.
The best solution for cancer cells.
